- Thyroid
Big Data Articles (National Health Insurance Service Database)
- Prevalence, Treatment Status, and Comorbidities of Hyperthyroidism in Korea from 2003 to 2018: A Nationwide Population Study
-
Hwa Young Ahn, Sun Wook Cho, Mi Young Lee, Young Joo Park, Bon Seok Koo, Hang-Seok Chang, Ka Hee Yi
-
Endocrinol Metab. 2023;38(4):436-444. Published online July 12, 2023
-
DOI: https://doi.org/10.3803/EnM.2023.1684
-
-
1,813
View
-
127
Download
-
1
Web of Science
-
3
Crossref
-
 Abstract Abstract
 PDF PDF Supplementary Material Supplementary Material PubReader PubReader  ePub ePub
- Background
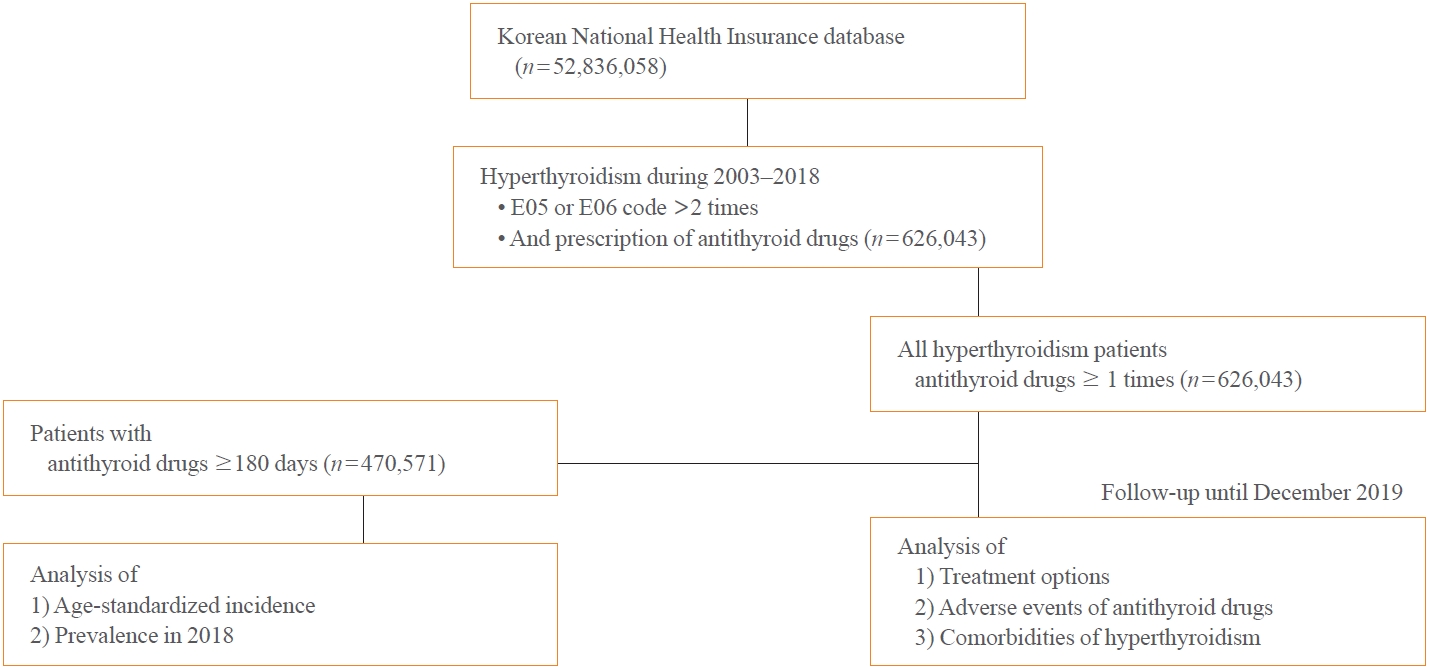
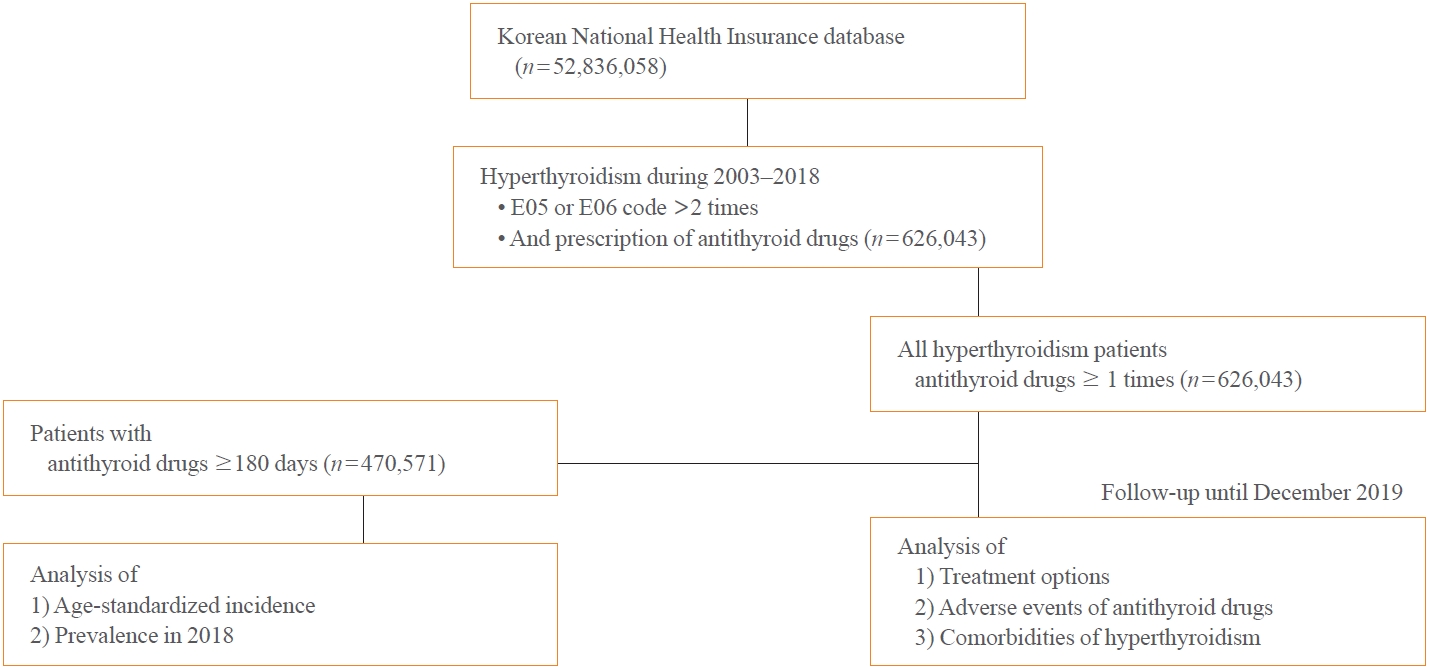
This study aimed to investigate the changes of incidence and treatment of choice for hyperthyroidism from 2003 to 2018 and explore the treatment-related complications and concomitant comorbidities in South Korea using data from the National Health Insurance Service.
Methods
This is a retrospective observational study. Hyperthyroidism was defined as a case having two or more diagnostic codes of thyrotoxicosis, with antithyroid drug intake for more than 6 months.
Results
The average age-standardized incidence of hyperthyroidism from 2003 to 2018 was 42.23 and 105.13 per 100,000 men and women, respectively. In 2003 to 2004, hyperthyroidism was most often diagnosed in patients in their 50s, but in 2017 to 2018, people were most often diagnosed in their 60s. During the entire period, about 93.7% of hyperthyroidism patients were prescribed with antithyroid drugs, and meanwhile, the annual rates of ablation therapy decrease from 7.68% in 2008 to 4.56% in 2018. Antithyroid drug-related adverse events, mainly agranulocytosis and acute hepatitis, as well as complications of hyperthyroidism such as atrial fibrillation or flutter, osteoporosis, and fractures, occurred more often in younger patients.
Conclusion
In Korea, hyperthyroidism occurred about 2.5 times more in women than in men, and antithyroid drugs were most preferred as the first-line treatment. Compared to the general population, hyperthyroid patients may have a higher risk of atrial fibrillation or flutter, osteoporosis, and fractures at a younger age.
-
Citations
Citations to this article as recorded by  - Long-term effect of thyrotropin-binding inhibitor immunoglobulin on atrial fibrillation in euthyroid patients
Jung-Chi Hsu, Kang-Chih Fan, Ting-Chuan Wang, Shu-Lin Chuang, Ying-Ting Chao, Ting-Tse Lin, Kuan-Chih Huang, Lian-Yu Lin, Lung-Chun Lin
Endocrine Practice.2024;[Epub] CrossRef - The Current Status of Hyperthyroidism in Korea
Hyemi Kwon
Endocrinology and Metabolism.2023; 38(4): 392. CrossRef - Is Thyroid Dysfunction Associated with Unruptured Intracranial Aneurysms? A Population-Based, Nested Case–Control Study from Korea
Hyeree Park, Sun Wook Cho, Sung Ho Lee, Kangmin Kim, Hyun-Seung Kang, Jeong Eun Kim, Aesun Shin, Won-Sang Cho
Thyroid®.2023; 33(12): 1483. CrossRef
- Clinical Study
- Association between Serum Gamma-Glutamyltransferase and Prevalence of Metabolic Syndrome Using Data from the Korean Genome and Epidemiology Study
-
Mi Young Lee, Dae Sung Hyon, Ji Hye Huh, Hae Kyung Kim, Sul Ki Han, Jang Young Kim, Sang Baek Koh
-
Endocrinol Metab. 2019;34(4):390-397. Published online December 23, 2019
-
DOI: https://doi.org/10.3803/EnM.2019.34.4.390
-
-
5,946
View
-
120
Download
-
14
Web of Science
-
14
Crossref
-
 Abstract Abstract
 PDF PDF PubReader PubReader  ePub ePub
- Background
The aim of this study was to determine whether there is a positive correlation between gamma-glutamyltransferase (GGT) levels and the prevalence of metabolic syndrome and whether GGT can be used as an easily checkable metabolic index using data from the large-scale Korean Genome and Epidemiology Study (KoGES). MethodsWe obtained data of 211,725 participants of the KoGES. The collected data included age, sex, height, weight, waist circumference, and various biochemical characteristics, including serum GGT levels. The data of study participants who ingested more than 40 g/day of alcohol and who were diagnosed with metabolic syndrome at baseline was excluded. We analyzed the prevalence of metabolic syndrome according to GGT quartiles in both genders. ResultsThe GGT level was significantly higher in subjects with metabolic syndrome compared to normal subjects (37.92±48.20 mg/dL vs. 25.62±33.56 mg/dL). The prevalence of metabolic syndrome showed a stepwise increase with GGT quartiles in both male and female subjects. Compared to the lowest GGT quartile, the odds ratio was 1.534 (95% confidence interval [CI], 1.432 to 1.643), 1.939 (95% CI, 1.811 to 2.076), and 2.754 (95% CI, 2.572 to 2.948) in men and 1.155 (95% CI, 1.094 to 1.218), 1.528 (95% CI, 1.451 to 1.609), and 2.022 (95% CI, 1.921 to 2.218) in women with increasing GGT quartile. The cutoff value of GGT predicting risk of metabolic syndrome was 27 IU/L in men and 17 IU/L in women. ConclusionWe suggested that GGT could be an easily checkable marker for the prediction of metabolic syndrome.
-
Citations
Citations to this article as recorded by  - Associating Liver Enzymes and Their Interactions with Metabolic Syndrome Prevalence in a Japanese Working Population
Aziz Jamal, Akira Babazono, Ning Liu, Rieko Yamao, Takako Fujita, Sung-a Kim, Yunfei Li
Metabolic Syndrome and Related Disorders.2024; 22(1): 27. CrossRef - Liver fat content assessed by conventional B-mode ultrasound and metabolic profile in non-diabetic patients: Implications for clinical practice
Rosanna Villani, Grazia Pia Magnati, Giulia Tuccari, Moris Sangineto, Antonino Davide Romano, Tommaso Cassano, Gaetano Serviddio
Ultrasound.2023; 31(3): 177. CrossRef - Serum γ-glutamyltransferase level and incidence risk of metabolic syndrome in community dwelling adults: longitudinal findings over 12 years
Jiwon Kwak, In-Ho Seo, Yong-Jae Lee
Diabetology & Metabolic Syndrome.2023;[Epub] CrossRef - Gamma-Glutamyl Transferase as a Diagnostic Marker of Metabolic Syndrome
Bobbili Tarun Kesava Naidu, Kakarlapudi Santosh Raju, Janapareddi V BhaskaraRao, Nallapati Sunil Kumar
Cureus.2023;[Epub] CrossRef - Metabolic syndrome and transaminases: systematic review and meta-analysis
Elena Raya-Cano, Rafael Molina-Luque, Manuel Vaquero-Abellán, Guillermo Molina-Recio, Rocío Jiménez-Mérida, Manuel Romero-Saldaña
Diabetology & Metabolic Syndrome.2023;[Epub] CrossRef - Association between Serum Gamma-glutamyl Transferase and Metabolic Syndrome: A Case–control Study
Akshay Shelar, Nalini Humaney, Akshay Chhajed, Krunal Domki, Ajay Narwade
Journal of Datta Meghe Institute of Medical Sciences University.2023; 18(4): 651. CrossRef - “Big Data” Approaches for Prevention of the Metabolic Syndrome
Xinping Jiang, Zhang Yang, Shuai Wang, Shuanglin Deng
Frontiers in Genetics.2022;[Epub] CrossRef - Can Gamma-glutamyl Transferase Predict Unhealthy Metabolic Phenotypes Among Healthcare Workers in Azar Cohort Study?
Mohammadhossein Somi, Seyed Sina Zakavi, Alireza Ostadrahimi, Negin Frounchi, Neda Gilani, Sarvin Sanaie, Elnaz Faramarzi
Hepatitis Monthly.2022;[Epub] CrossRef - Association between liver enzymes and metabolic syndrome in Canadian adults: results from the Canadian health measures survey - cycles 3 &4
Luan Manh Chu, Chandima Karunanayake, Palok Aich, Markus Hecker, Punam Pahwa
Journal of Diabetes & Metabolic Disorders.2022; 21(2): 1699. CrossRef - Repeatedly elevated γ-glutamyltransferase levels are associated with an increased incidence of digestive cancers: A population-based cohort study
Chang-Hoon Lee, Kyungdo Han, Da Hye Kim, Min-Sun Kwak
World Journal of Gastroenterology.2021; 27(2): 176. CrossRef - Index of Cardiac Age Index and Cardiometabolic Biomarkers in Adults with Metabolic Syndrome
Eun Jung Choi, Sang Yeoup Lee
Metabolic Syndrome and Related Disorders.2021; 19(5): 288. CrossRef - Simple metabolic markers associated with tophaceous gout
Wei Liu, Hui Song, Siliang Man, Hongchao Li, Siming Gao
Clinical Rheumatology.2021; 40(12): 5047. CrossRef - Expression Status and Prognostic Significance of Gamma-Glutamyl Transpeptidase Family Genes in Hepatocellular Carcinoma
Shan Tian, Jiao Li, Yingyun Guo, Weiguo Dong, Xin Zheng
Frontiers in Oncology.2021;[Epub] CrossRef - Nonalcoholic fatty liver disease and the risk of insulin-requiring gestational diabetes
Sang Youn You, Kyungdo Han, Seung-Hawn Lee, Mee Kyoung Kim
Diabetology & Metabolic Syndrome.2021;[Epub] CrossRef
- A Case of Primary Hyperparathyroidism Associated with Gall-bladder Stone and Chronic Cholecystitis.
-
Jin Hyung Lee, Pil Moon Jung, Chong Whan Kim, Myeong Sang Shin, Hong Jun Park, Soo Min Nam, Mi Young Lee, Jang Hyun Koh, Mee Yoen Cho, Jang Yel Shin, Choon Hee Chung, Young Goo Shin
-
J Korean Endocr Soc. 2007;22(6):470-474. Published online December 1, 2007
-
DOI: https://doi.org/10.3803/jkes.2007.22.6.470
-
-
 Abstract Abstract
 PDF PDF
- Primary hyperparathyroidism is caused mainly by a parathyroid adenoma or hyperplasia, and is characterized by hypercalcemia and hypophosphatemia induced by an increased level of parathyroid hormone (PTH). Patients with primary hyperparathyroidism are usually asymptomatic and the disease is most often detected incidentally. However, patients can present with symptoms of renal stones, peptic ulcer disease, muscle weakness, depression, constipation, and pancreatitis. In addition, it has been reported that choletithiasis can be combined with primary hyperparathyroidism. We report a case of a 49-year-old man with primary hyperparathyroidism accompanied with chronic cholecystitis caused by a gallbladder (GB) stone. The chief complaint was nausea, poor oral intake, abdominal pain, and weight loss. Abdominal sonography was performed and chronic cholecystitis with a GB stone was diagnosed. The serum calcium level was 18.5 mg/dL and the intact parathyroid hormone level was 1,777 pg/mL. A parathyroid mass was detected by neck-computed tomography, neck ultrasonography and a (99m)Tc-Tetrofosmin parathyroid scan. The parathyroid mass was removed and the mass was confirmed as a parathyroid adenoma. Cholecystectomy was performed and the diagnosis of chronic cholecystitis was confirmed. After the surgical procedure, the symptoms improved and the calcium level was normalized.
- A Case of Graves' Disease with Ulcerative Colitis.
-
Pil Moon Jung, Mi Young Lee, Jang Hyun Koh, Jang Yeol Shin, Young Goo Shin, Mi Yeion Jo, Choon Hee Chung
-
J Korean Endocr Soc. 2007;22(2):149-152. Published online April 1, 2007
-
DOI: https://doi.org/10.3803/jkes.2007.22.2.149
-
-
 PDF PDF
- A Case of Adrenal Incidentaloma with a Pituitary Incidentaloma.
-
Myoung Kyu Lee, Su Min Nam, Jang Hyoun Ko, Mi Young Lee, Jang Yeol Sin, Kwang Wha Park, Choon Hee Chung
-
J Korean Endocr Soc. 2006;21(6):577-582. Published online December 1, 2006
-
DOI: https://doi.org/10.3803/jkes.2006.21.6.577
-
-
 Abstract Abstract
 PDF PDF
- Incidentaloma is defined as an asymptomatic mass lesion that shows no associated hormonal hyper- or hyposecretion. Adrenal incidentaloma is also a typical mass detection of which is known to have increased with improved imaging techniques such as CT or MRI. We report a case in which a pituitary incidentaloma is accompanied by an adrenal incidentaloma. The 65-year-old patient was admitted due to oropharyngeal pain, and had a medical history that included an operation for rectal cancer. The adrenal tumor had no function, but left adrenalectomy was performed for the evaluation of rectal cancer recurrence, which was diagnosed pathologically as a benign adrenocortical nodule. In our experience we have found that, in the case of multiple incidentalomas, it is important to evaluate the function or malignancy status of each.
- A Case of Iodine-induced Thyrotoxicosis with Acromegaly.
-
Kwang Hyun Kim, Kyu Hong Kim, Ho Yoel Ryu, Su Min Nam, Mi Young Lee, Jang Hyun Koh, Jang Yeol Sin, Choon Hee Chung
-
J Korean Endocr Soc. 2006;21(1):63-67. Published online February 1, 2006
-
DOI: https://doi.org/10.3803/jkes.2006.21.1.63
-
-
 Abstract Abstract
 PDF PDF
- Hyperthyroidism is seen in 3.5-26% of subjects with acromegaly. Hyperthyroidism can be developed by thyroid stimulating hormone (TSH) dependent mechanism in TSH-secreting adenomas with acromegaly or by TSH independent mechanism through the stimulation of thyroid cells by growth hormone (GH). So, confirming the cause of hyperthyroidism is important to treat that. We report a case of a 56-year-old man who had acromegaly with iodine-induced thyrotoxicosis. He took the sea tangle for 4 years because he had constipation. His face and hands indicated acromegaly. Thyroid function test showed that T3 and free T4 were increased and TSH was decreased. Ultrasonography of neck showed diffuse enlargement of thyroid gland and thyroid scan showed decreased uptake of thyroid gland. So we could confirm iodine-induced thyrotoxicosis due to excessive iodine intake. Serum GH and insulin-like growth factor (IGF)-1 were markedly increased and brain MRI showed heterogenous 1 cm sized pituitary mass in right side. Acromegaly was confirmed by brain MRI, pituitary stimulation test and increased level of GH, IGF-1. He stopped iodine intake. After 6 months, T3, free T4 and TSH were normalized and he is waiting for the surgical removal of pituitary adenoma.
- A Case of Adrenocortical Adenoma Causing Subclinical Cushing's Syndrome Mistaken for Liddle's Syndrome.
-
Kyu Hong Kim, Kwang Hyun Kim, Ho Yoel Ryu, Soo Min Nam, Mi Young Lee, Jang Hyun Koh, Jang Yel Shin, Soon Hee Jung, Choon Hee Chung
-
J Korean Endocr Soc. 2006;21(1):58-62. Published online February 1, 2006
-
DOI: https://doi.org/10.3803/jkes.2006.21.1.58
-
-
2,085
View
-
25
Download
-
1
Crossref
-
 Abstract Abstract
 PDF PDF
- Subclinical Cushing's syndrome is defined as an autonomous cortisol hyperproduction without specific clinical signs of cortisol excess, but detectable biochemically as derangements of the hypothalamic-pituitary-adrenal axis function. We report a case of a 33-year-old woman with subclinical Cushing's syndrome caused by left adrenocortical adenoma, mistaken for Liddle's syndrome. The patient complained of fatigue. Laboratory findings showed metabolic alkalosis, hypokalemia, high TTKG (transtubular K concentration gradient), low plasma renin activity, and low serum aldosterone level, that findings implied as Liddle's syndrome. So we performed further study. Hormonal and radiologic studies revealed subclinical Cushing's syndrome with a left adrenal mass. The adrenal mass was resected and pathologically diagnosed as adrenocortical adenoma. After the resection of the left adrenal mass, patient's hormonal levels showed normal range.
-
Citations
Citations to this article as recorded by  - Missed Ipsilateral Adrenal Adenoma With Recurrent Hypercortisolism After Prior Left Adrenalectomy
Jihoon Kim, Hae Kyung Kim, Choon Hee Chung
Journal of Korean Medical Science.2022;[Epub] CrossRef
- A Case of Drug Induced Nephrogenic Diabetes Insipidus and Hyperprolactinemia in Schizophrenia Simultaneously.
-
Ho Yoel Ryu, Mi Young Lee, Yeon Lee, Jang Hyun Koh, Mi Jin Kim, Young Goo Shin, Choon Hee Chung
-
J Korean Endocr Soc. 2005;20(4):407-412. Published online August 1, 2005
-
DOI: https://doi.org/10.3803/jkes.2005.20.4.407
-
-
 Abstract Abstract
 PDF PDF
- In schizophrenia, when treatment using antipsychotics fails, lithium, which is known as an antimanic drug, can also be administered. It is reported that 12~20% of patients taking lithium develop nephrogenic diabetes lactotrophs. Hyperprolactinemia is induced by typical antipsychotics, as they block the dopamine-2 receptors of latotrophs in the pituitary gland. Therefore, atypical antipsychotics for decreasing the side effect, such as hyperprolactinemia, can be used. However, hyperprolactinemia can be induced by risperidone, one of the atypical antipsychotics. Here, a case of drug induced nephrogenic diabetes insipidus and simultaneous hyperprolactinemia, which occurred in a patient with schizophrenia, is reported.
|